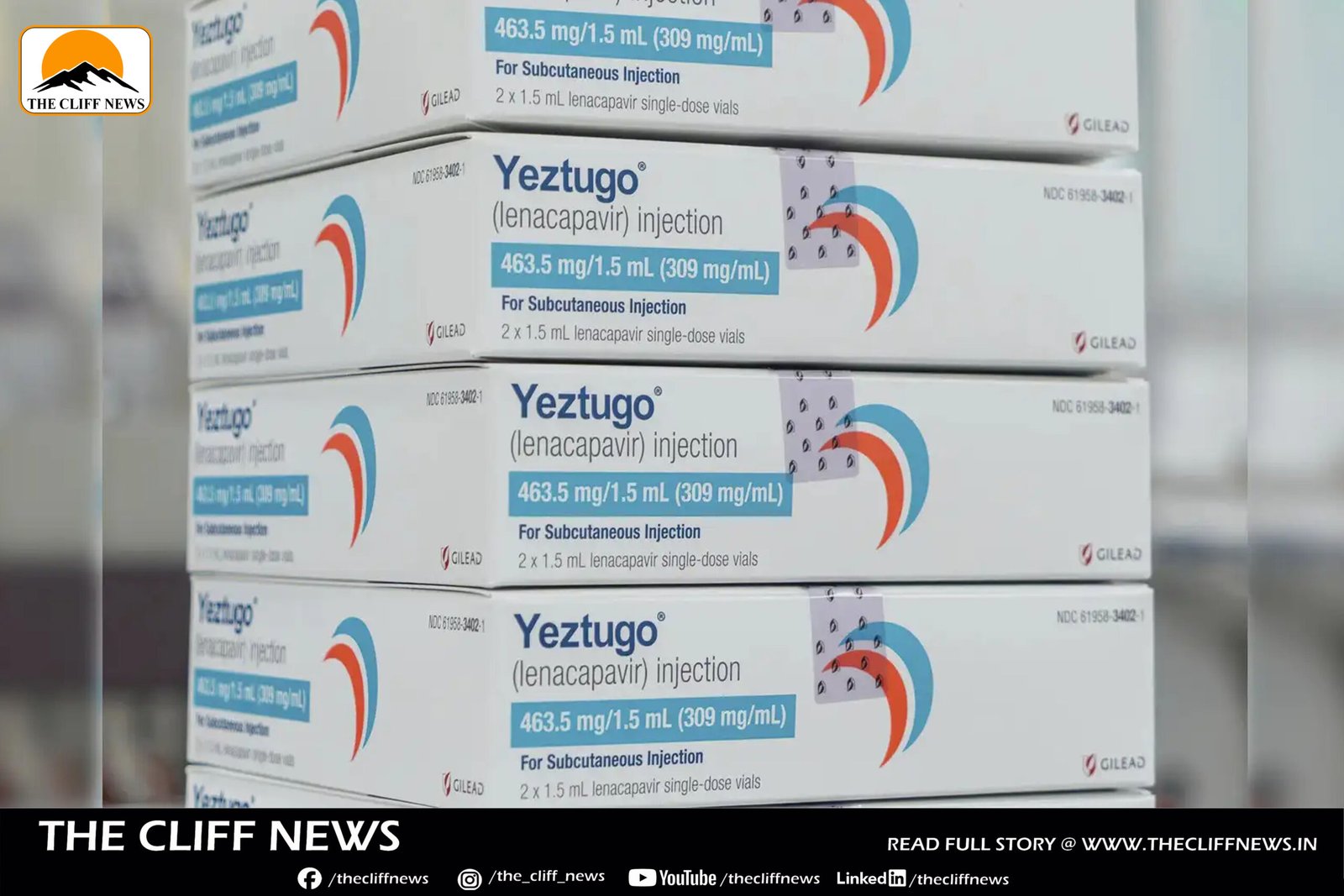
The U.S. Food and Drug Administration (FDA) has approved Gilead Sciences’ lenacapavir — a twice-yearly injectable drug to prevent HIV infection — in a move hailed as a historic breakthrough in the decades-long battle against the virus. Marketed under the brand name Yeztugo, the drug is the first twice-yearly pre-exposure prophylaxis (PrEP) treatment to receive FDA approval.
“This is a historic day in the decades-long fight against HIV,” said Daniel O’Day, Chairman and CEO of Gilead Sciences, following the announcement.
A Potential Game-Changer in HIV Prevention
Unlike previous PrEP options like Truvada, which require daily pills, Yeztugo offers a bi-annual injection that has demonstrated exceptional efficacy. In clinical trials involving over 4,000 participants:
- Among women in sub-Saharan Africa, the drug showed 100% protection.
- Among men and gender-diverse individuals, it showed a 99.9% prevention rate.
Only two infections were reported across all study participants. The results, published in The New England Journal of Medicine, earned lenacapavir the 2024 “Breakthrough of the Year” title by Science magazine.
Reported side effects included mild injection site reactions, headache, and nausea.
Affordability and Equity Concerns
Despite its promise, the $28,218 annual list price in the U.S. has raised significant concerns among activists, researchers, and public health experts, particularly those fighting for access in low- and middle-income countries.
Gilead spokesperson Blair Baumwell said the pricing is “in line” with other PrEP products, and the company expects broad insurance coverage to support access.
However, critics argue the pricing is a major obstacle.
“Even high-income countries will not be able to afford widespread use of lenacapavir at prices above $20,000 per year,” warned Andrew Hill, researcher at Liverpool University, who has shown that the drug could be mass-produced for as little as $25 per year.
Global Access Plans Underway
In an effort to expand global access, Gilead signed agreements in October 2024 with six pharmaceutical companies to manufacture generic versions of lenacapavir for 120 low- and middle-income countries, pending regulatory approvals.
Additionally, a separate deal with the Global Fund, the UN, and PEPFAR (President’s Emergency Plan for AIDS Relief) aims to supply the drug to 2 million people. However, budget cuts to PEPFAR under the Trump administration have cast doubt on the sustainability of this effort.
A Global Turning Point — If Accessible
UN Under-Secretary-General Winnie Byanyima emphasized the importance of equitable pricing:
“Lenacapavir could be the tool we need to bring new infections under control — but only if it is priced affordably and made available to everyone who could benefit.”
As the HIV/AIDS community celebrates this scientific milestone, pressure is now mounting on Gilead and global health institutions to ensure that cost doesn’t become a barrier to what could be a revolutionary tool in ending the HIV epidemic.